For millions of people living with inflammatory bowel disease, the search for relief often leads down a familiar path of medications, dietary restrictions, and invasive procedures. But groundbreaking research is revealing an unexpected ally in the fight against IBD—one that’s been hiding in plain sight within our own nervous system.
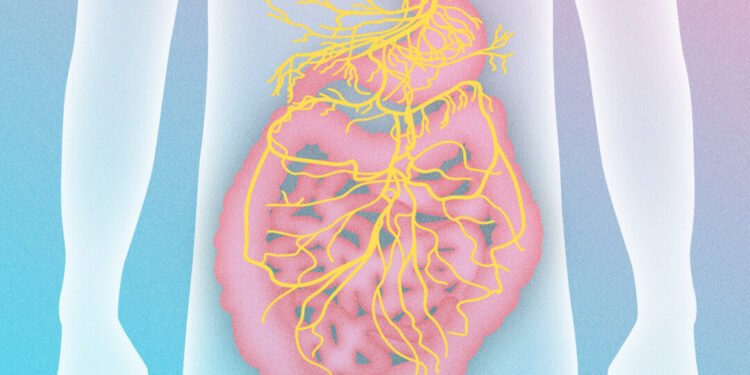
The vagus nerve, often called the body’s internal superhighway, connects our most vital organs directly to the brain. This remarkable neural pathway serves as the command center for our parasympathetic nervous system, orchestrating the crucial “rest-and-digest” functions that keep us healthy. Now, medical experts are discovering that learning to activate this powerful nerve could offer new hope for those battling the debilitating effects of inflammatory bowel disease.
The Missing Link in IBD Treatment
Inflammatory bowel disease encompasses both Crohn’s disease and ulcerative colitis, conditions characterized by chronic inflammation and painful ulcerations throughout the digestive tract. Traditional medical approaches have long relied on anti-inflammatory medications, immune-suppressing drugs, strict dietary modifications, and surgical interventions to manage symptoms.
However, a growing number of healthcare professionals are shifting their focus toward a more holistic understanding of IBD’s underlying mechanisms. At the center of this new perspective lies the vagus nerve—a critical component that many treatment protocols have historically overlooked.
When properly stimulated, the vagus nerve triggers a cascade of beneficial physiological responses. The body naturally transitions into a state of calm, systemic inflammation begins to subside, and digestive processes optimize themselves for healing. This creates an internal environment that’s not just conducive to managing IBD symptoms, but potentially reversing some of the damage caused by chronic inflammation.
Two Proven Pathways to Vagus Nerve Activation
Medical experts have identified two primary lifestyle approaches that can effectively stimulate vagus nerve function, offering IBD patients practical tools for managing their condition. These evidence-based methods don’t require expensive equipment or invasive procedures—instead, they harness the body’s natural healing mechanisms through targeted lifestyle modifications.
The first approach focuses on specific breathing techniques that directly influence vagus nerve activity. Deep, controlled breathing patterns can trigger the parasympathetic response, helping to calm inflammation throughout the digestive system. Research has shown that consistent practice of these breathing exercises can lead to measurable improvements in IBD symptoms over time.
The second pathway involves targeted physical activities and postural adjustments that enhance vagus nerve stimulation. These gentle but effective techniques work by improving the nerve’s ability to communicate between the gut and brain, facilitating better digestive function and reducing inflammatory responses.
A New Frontier in Digestive Health
This emerging understanding of the vagus nerve’s role in IBD represents a significant shift in how medical professionals approach digestive disorders. Rather than simply managing symptoms as they arise, this approach addresses one of the fundamental communication networks that govern intestinal health.
For patients who have struggled with limited success using conventional treatments alone, vagus nerve activation offers a complementary strategy that works with the body’s existing systems rather than against them. The beauty of this approach lies in its accessibility—these techniques can be learned and practiced by anyone, regardless of their current treatment regimen.
As research continues to unveil the complex relationships between our nervous system and digestive health, the vagus nerve is emerging as a powerful ally in the quest for IBD relief. By learning to harness this internal highway’s healing potential, patients may find themselves with new tools for reclaiming their digestive health and overall quality of life.
This breakthrough understanding doesn’t just offer hope for IBD sufferers—it represents a fundamental shift toward more integrated, patient-empowered approaches to managing chronic digestive conditions. As more people discover the transformative potential of vagus nerve activation, we may be witnessing the dawn of a new era in digestive health management.